Genetically modified neural stem cells showing promising therapeutic potential for spinal cord injury
A major advance in treating spinal cord injuries by using genetically modified human neural stem cells (hNSCs) has been made by a team co-led by City University of Hong Kong (CityU) and the University of Hong Kong (HKU).
Patients with spinal cord injuries often experience lifelong disabilities because of a lack of effective clinical management or treatment regimens. However, the CityU-HKU research team has discovered that modifying specific genes in hNSCs can alter their intrinsic actions, effectively driving nerve regeneration to repair damage and ultimately restoring locomotor functions. The finding offers excellent potential for new therapeutic opportunities for spinal cord injury.
Traumatic injuries to the spinal cord are often caused by falls, car crashes or sport-related incidents. Under normal circumstances, spinal neurons receive or transmit information to the brain through descending/ascending pathways. These pathways consist of long axons that transmit signals from the brain to the spinal cord or from the spinal cord to the brain, where active synaptic interactions among neurons control our movement and sensory perception. Spinal cord injuries cause irreversible damage to neurons and axons, which can significantly interrupt signal transmission, leading to defective locomotion and somatosensory functions.

“While recent progress has been made in promoting spinal cord repairs through the transplantation of hNSCs derived from human induced pluripotent stem cells (iPSCs), the degree of functional recovery obtained has been modest. This is largely due to the hostile micro-environment around the lesion site, such as the formation of barrier-like structures called astroglial scars and the lack of neurotrophic factors in adults for neuronal differentiation. These factors hinder functional neuronal regeneration, resulting in prolonged or limited functional recovery,” explained Professor Jessica Liu Aijia, Department of Neuroscience (NS) at CityU and the co-leader of the research.
The “deleterious” gene SOX9 was reported to have had a high-level expression at the injury site, while the gene itself is the leading cause of glial scars and the hindrance of neuronal survival and differentiation. The joint-research team found that modifying the expression of the SOX9 gene in hNSCs by approximately 50% can effectively enhance the survival and neuronal differentiation potential of hNSCs in a hostile microenvironment, promoting neural circuits reconstruction in the spinal cord within a shorter period.
To further explore the therapeutic effects of SOX9-gene-modified hNSCs in treating SCI, the team used a severe spinal cord injury rat model and conducted various behaviour tests, including grid walking and consecutive walk, to evaluate locomotion recovery after transplantation. The grid walking test examines the rats' ability to coordinate their limbs, such as whether they could correctly place their left and right front and hind paws on the grid and then grip. The consecutive walk test evaluates the rats' stepping patterns to assess their gait and fingertip motor ability.
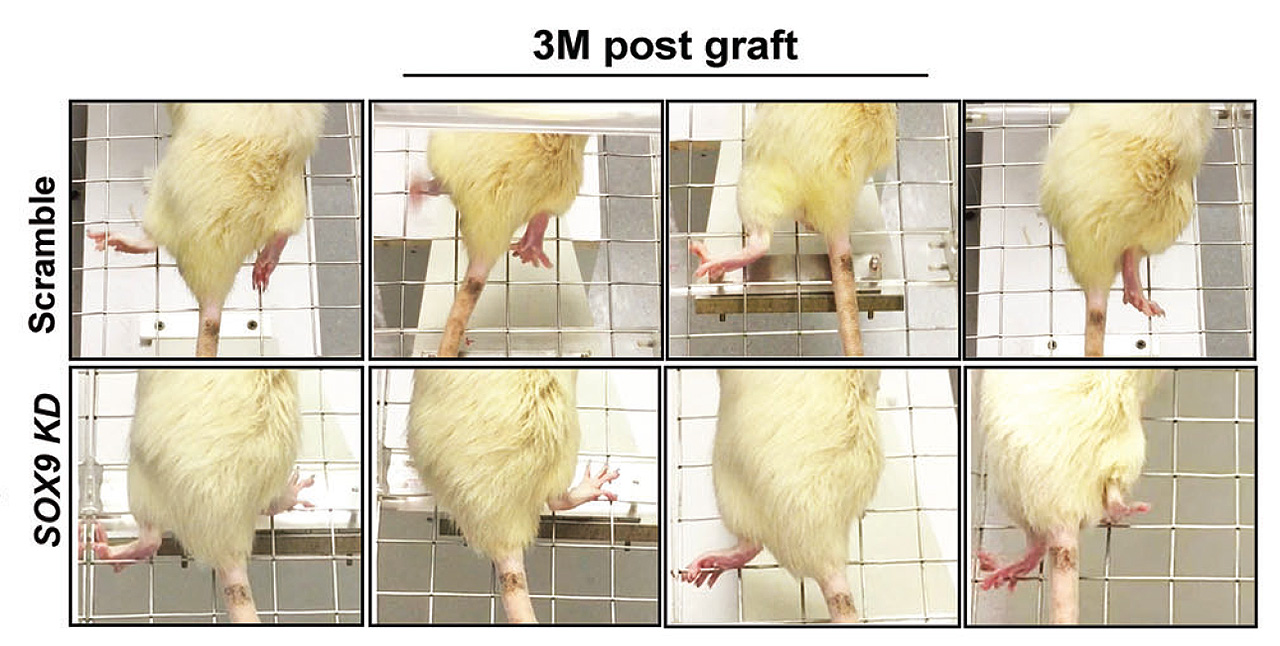
Compared to rats grafted with non-modified hNSCs, rats grafted with SOX9 gene-modified hNSCs performed much better, placing their affected hind paws on the grid with fewer misdirected steps after ten weeks post-injury. In addition, these treated rats also demonstrated an excellent gait with clear paw position and toe movement when walking across a metre-long narrow corridor.
“Our study uses genetic modification to alter the response of hNSCs to the deleterious microenvironment in vivo after injury, improving cell tolerance to the niche and self-differentiation potential. This brings a new treatment direction for repairing damaged spinal cord,” said Professor Liu.
“This modified hNSCs derived from iPSCs, which can be generated from a patient's skin or blood cells, eliminates ethical concerns in using embryonic stem cells and minimises the risk of a rejection by the immune system,” she added.
The paper's first co-authors and the corresponding authors are Professor Liu and Dr Martin Cheung Chi-hang, Associate Professor, School of Biomedical Sciences, Li Ka Shing Faculty of Medicine, HKU (HKUMed). The other collaborators include Professor Chan Ying-shing of HKUMed and researchers at CityU. The research has been funded by the Research Grants Council, Hong Kong.